Slowing Dewormer Resistance
By Susan Schoenian, Sheep 101
Dewormer resistance is inevitable, but the rate at which it develops is not.
It is a well-known fact that gastro-intestinal parasites (worms) have developed resistance to all of the currently available dewormers (anthelmintics).[1,2,8] Resistance means that an anthelmintic treatment is not effective (or only marginally effective) at killing worms and alleviating clinical symptoms. Worm resistance is heritable; the worm’s ability to survive is passed onto its offspring.
Resistance may result in deaths and/or production losses. It varies by species, geographic region, and farm, but is the worst in small ruminants and in warm, moist climates where parasites are more endemic.
Dewormer resistance is inevitable, but the speed at which it develops is not. For many producers, the level of resistance is still at a level at which there is time to slow it down and enable the continued use of anthelmintics.
The primary cause of today’s dewormer resistance is frequent deworming, especially without regard to clinical need. The practice of deworming small ruminants based on some arbitrary schedule (e.g. every three months) or because they have some worm eggs in their feces is outdated and never was a good idea, certainly not a sustainable one.
The improper use of dewormers has also accelerated the development of drug-resistant worms. Underdosing is especially problematic because it delivers a sub-therapeutic dose to the animal, making it easier for the worms to develop resistance. Sub-therapeutic doses also result when a dewormer is poured on the animal’s back or injected into its body.
Pour-on dewormers were not developed for sheep and goat skin, hair, or wool. Their active ingredient is not going to be absorbed as well. Injectable dewormers do not immediately clear the animal’s system. They leave a drug residual, making it easier for the worms to develop resistance. In addition, there are no pour-ons or injectable dewormers that are FDA-approved for use in sheep and/or goats (in the United States).
Dewormers with “persistent activity” (macrocylic lactones) also increase selection for resistant worms, as the worms are being exposed to a sub-therapeutic level of drug. Worms that are exposed to sub-therapeutic levels of drugs may not survive if they were otherwise exposed to a full dose of the drug.
Certain management practices can accelerate the development of resistant worms. Moving treated animals to a clean pasture is no longer a recommended practice because the only surviving worms (eggs, larvae) will be resistant to the dewormer that was just used. Animals should not be dewormed when the level of infection is low. For example, very few females will have a heavy parasite load pre-breeding. Thus, deworming at this time will increase selection for resistant worms. Deworming when pasture contamination is low (e.g. during a drought), will increase the proportion of resistant worms in the population.
Proper use of dewormers
The first step in slowing drug resistance is understanding the drugs and knowing which ones work on your farm. While there are numerous dewormers on the market, there are only three anthelmintic classes in which they fit. Anthelmintics in the same drug class have a similar mode of action. Resistance is to the mode of action, not the drug. Thus, cross-resistance occurs among drugs in the same anthelmintic class. The more potent drugs in a class (e.g. albendazole, moxidectin and levamisole) may initially be more effective, but resistance will develop more quickly than if the drug was from a different anthelmintic class.
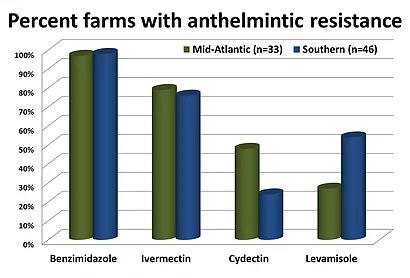
The oldest class of anthelmintics is the benzimidazoles (BZD), commonly called “white” dewormers or drenches. This class includes fenbendazole, albendazole, and oxfendazole. It makes sense that resistance to the benzimidazoles is usually highest, as they’ve been in use for the longest period of time.
The macrocylic lactones (ML) are the newest anthelmintic class, though the last drug (moxidectin) was introduced in 1997 and ivermectin has been around for more than 25 years. The MLs consist of two sub-classes: the avermectins and milbimycins. Moxidectin is a more potent drug than ivermectin and will initially kill ivermectin-resistant worms, but resistance to it is growing rapidly.[1] The macrocylic lactones have “persistent activity,” which means they remain in the system longer.
The third group of anthelmintics is called nicotinic agonists, so-named for their method of killing worms. It includes levamisole, morantel, and pyrantel. Though levamisole has been around for a long time, resistance to it is slower to develop than other drugs, which may explain why it is still effective on some farms. It was also unavailable for a few years. Morantel is administered in feed. Pyrantel is used less frequently by small ruminant producers.
Targeted Selective Treatments (TST)
The primary way to slow dewormer resistance is to reduce the number of anthelmintic treatments. To do so, targeted selective treatment (TST) strategies need to be employed. TST identifies those animals which require treatment and/or those animals which would benefit from treatment. Rarely should the whole flock or herd be treated for internal parasites. Nor should anthelmintic treatments be scheduled using a calendar. Instead, individual deworming decisions should be made on the basis of FAMACHA© (eye anemia) scores and other criteria.
The Five Point Check© is an extension of the FAMACHA© system.[5] It is a decision-making tool that allows farmers to make deworming decisions for all of the parasites that commonly affect small ruminants.[5] Developed by researchers in South Africa, the Five Point Check© involves five check points on the animal: ocular mucous membranes (FAMACHA© score) back (body condition score), tail (dag score), jaw (bottle jaw), and nose (nasal discharge). The Five Point Check© was developed for sheep. For goats, it is suggested that the nose check point be replaced with coat condition (or appearance), as nasal bots tend to be less problematic in goats than sheep.
Weight gain is another criteria that can be used to determine which animals would benefit from deworming. For example, the heaviest lambs or kids can be left untreated, assuming they are of similar breed and age. In Scotland, researchers based deworming decisions on target weights.[9] By doing so, they were able to maintain weight gains and reduce the number of animals that required deworming, while preserving the effectiveness of the anthelmintic.
Fecal egg counting
Individual fecal tests, especially qualitative analyses, are not recommended for diagnostic purposes. In fact, the diagnostic test for the barber pole worm (the primary worm parasite in warm, moist climates) is a blood test: packed cell volume (PCV). A sheep or goat that has worm eggs in its feces or even a high fecal egg count does not necessarily need dewormed and vice versa. Plus, it is difficult to determine what egg count is of clinical significance, as there are so many factors which affect egg counts and an animal’s susceptibility to worm infection.
On the other hand, fecal egg counts (FECs) and (and should) be used to monitor pasture contamination, test for drug resistance, and/or identify resistant (or susceptible) animals. In large flocks or situations where the barber pole worm is not the primary parasite, fecal egg counts can help pinpoint the need for deworming.
The effectiveness of an anthelmintic can be determined by comparing before and after fecal egg counts. This is called a fecal egg count reduction test (FECRT). A fecal sample (> 200 epg) is collected at the time of deworming. A second sample is collected from the same animal 7 to 14 days later. The percent reduction in fecal egg count is calculated and compared to a group of “control” animals that were not dosed. An effective deworming should reduce fecal egg counts by 95 percent or more. A high level of resistance is present if egg counts are reduced by less than 60 percent.
The DrenchRite® test (larval development assay) can also be used to detect drug resistance.[3] The DrenchRite® test utilizes eggs isolated from the feces of infected animals and tests for resistance to all drugs simultaneously. A pooled fecal sample (>350-500 epg) from at least 10 animals is required. The DrenchRite® test can also be used to identify worm species.[3]
Drenching
Another way to slow dewormer resistance is to avoid underdosing and exposing worms to sub-therapeutic levels of the dewormer. To avoid underdosing, animals should be weighed and given doses that are appropriate for their weight and species. Goats usually require higher doses of anthelmintics than sheep and other livestock because they metabolize the drugs more quickly. In fact, it is common to give goats 1.5 to 2 times the sheep (or cattle) dose of an anthelmintic, with the 1.5 dose being for levamisole, the anthelmintic with the narrowest margin of safety.

Sheep and goats should always be dewormed with drench (liquid) formulations. Drenches are FDA-approved, safer, and generally more effective[4] than other formulations. Oral medications also have shorter withdrawal periods. For example, the withdrawal period for a subcutaneous injection of moxidectin (Cydectin®) is 132 days in goats, whereas the withdrawal period for the oral drench is only 17 days (goats).[7]
Sheep and goats should be dewormed using an oral dosing syringe with a long, metal nozzle. The syringe can be a single dose syringe or an automatic syringe that refills after each treatment. If an automatic (backpack) drench gun is used, the equipment should be calibrated for the heaviest animals in the group not the average. Drenching equipment should be regularly checked to make sure it is delivering the desired level of medicine.
The drug should be deposited over the tongue into the esophagus. If the medicine is deposited into the animal’s mouth, this may stimulate the closure of the esophageal groove, causing the medicine to bypass the rumen and be less effective. Fasting animals prior to drenching can also increase the effectiveness of certain dewormers (e.g. benzimidazoles, ivermectin).[6] Another strategy is to give two consecutive doses 12 hours apart.[6] The longer the drug is in the rumen, the more effective it will be
It goes without saying that all drugs should be used according to the manufacturer’s instructions. Anthelmintics that are not properly stored may be less effective. Anthelmintics should not be left in the barn, but should be stored at a constant temperature, ideally in a refrigerator. While no one likes to discard expensive medicines, outdated drugs may be less effective and thus contribute to the development of resistant worms. Drugs should never be mixed.
Quarantine drenching
Because newly purchased animals can be as source of anthelmintic resistance, all new arrivals should be kept in a quarantine pen and be dewormed with drugs from two (levamisole + moxidectin) or three (albendazole + levamisole + moxidectin) anthelmintic classes. The idea is to kill all the worms so that no resistant worms survive, as worms pass resistant genes onto their offspring.
Leaving some animals untreated and/or keeping animals on the same pasture will help to dilute the worm populations and maintain “refugia” (untreated worms). Maintaining refugia is the key to slowing drug resistance. If you treat at pre-breeding, pre-lambing, or post-weaning, be sure to leave some animals untreated. Another good option is to keep livestock in the barn or drylot for 24 to 48 hours after treatment with an anthelmintic. This will ensure than any eggs that are present in the gut have passed out into the feces.
Of course, any practice that reduces the need for deworming will slow drug resistance. Rotational grazing can reduce or increase the need for deworming, depending upon how it is practiced. The keys are not allowing pastures to become too contaminated with infective worm larvae and allowing sufficient rest periods to enable worm eggs and larvae to die off. Removing a hay or silage crop will result in a clean pasture for grazing. Co-grazing small ruminants with cattle or horses can have beneficial effects on both pasture and parasite management.
Maintaining a sufficient grazing height of at least 3-4 inches will reduce ingestion of infective worm larvae, as it is estimated that approximately 80 percent of worm larvae is in the first two inches of vegetative growth. Along the same line, animals that browse will be exposed to less infective worm larvae. Some forages (e.g. Sericea lespedeza, chicory) have been shown to inhibit parasite development. Zero grazing will obviously reduce (if not eliminate) the need for deworming; however, it will prevent animals from developing immunity.
Genetic selectionSpecies, breeds and individuals within a breed differ in their ability to handle parasitic infection. Goats tend to be more susceptible to parasites than sheep. Hair sheep (e.g. St. Croix, Barbado) are more resistant to parasites than their woolly counterparts. The resistance of hair x wool crosses (e.g. Katahdin) tends to be intermediate between hair and wooled breeds. The Gulf Coast Native is the only wooled breed of sheep with documented parasite resistance.
While less data is available on goats, Kiko, Spanish, and Myotonic goats tend to be more resistant to parasites than Boers, Nubians, and other breeds. Though the level of heterosis has not been documented, crossbred individuals will tend to be more parasite-resistant than their purebred counterparts.
Any flock or herd can be selected for reduced parasite infection. Parasites are not evenly dispersed in a flock or herd. The 80-20 rule states that 20 percent of the animals are responsible for 80 percent of the worm infection (fecal egg counts). By selecting animals that shed fewer eggs and require less frequent anthelmintic treatments, a producer can reduce anthelmintic use and slow drug resistance, while developing a more resistant herd.
Parasite resistance, as quantified by fecal egg counts, is a moderately heritable trait. Parasite resilience, as quantified by packed cell volumes (and estimated by FAMACHA© scores) is less heritable, but correlated to parasite resistance
The most important strategy is to use a ram or buck that has documented resistance to internal parasites. Unfortunately, selection programs for resistant sheep and goats are still in their infancy. The Katahdin breed is the only breed (in the U.S.) in which EBV’s are calculated (via LambPlan) for parasite resistance (fecal egg counts). The primary goal of the Western Maryland Pasture-Based Meat Goat Performance Test is to identify bucks that are both resistant and resilient to internal parasites. Virginia Tech’s Southwest AREC’s hair sheep ram test includes an evaluation for parasite resistance.
A new anthelmintic[11]
There is a new anthelmintic called Zolvix® (monepantel). It is the first anthelmintic in a new class of anthelmintics called Amino-Acetonitrile Derivatives (ADD). Zolvix® is effective against the worms that are resistant to the other anthelmintic classes. However, like all dewormers, resistance to Zolvix® is inevitable. In fact, resistance may already have been detected in a hobby herd of goats in New Zealand.
Zolvix® is available in most countries, but not yet the United States, where it is awaiting FDA approval. When Zolvix® becomes available, it needs to be used in a manner that preserves its effectiveness for as long as possible. Resistance is inevitable, but the rate at which it develops is not.

About the Author
Susan Schoenian is the Sheep & Goat Specialist at the University of Maryland’s Western Maryland Research & Education Center in Keedysville, Maryland. She has been with University of Maryland Extension since 1988. Susan began her extension career as an agricultural extension agent (“county agent”) in Wicomico County, Maryland. She also served as a Farm Management Specialist for Maryland’s nine Eastern Shore counties. In addition, she operates the following websites: Sheep 101, Sheep 201 and Maryland Small Ruminant Page, and Wormx.
References and suggested additional reading:
This article was written in 2013 by Susan Schoenian.

